Overview
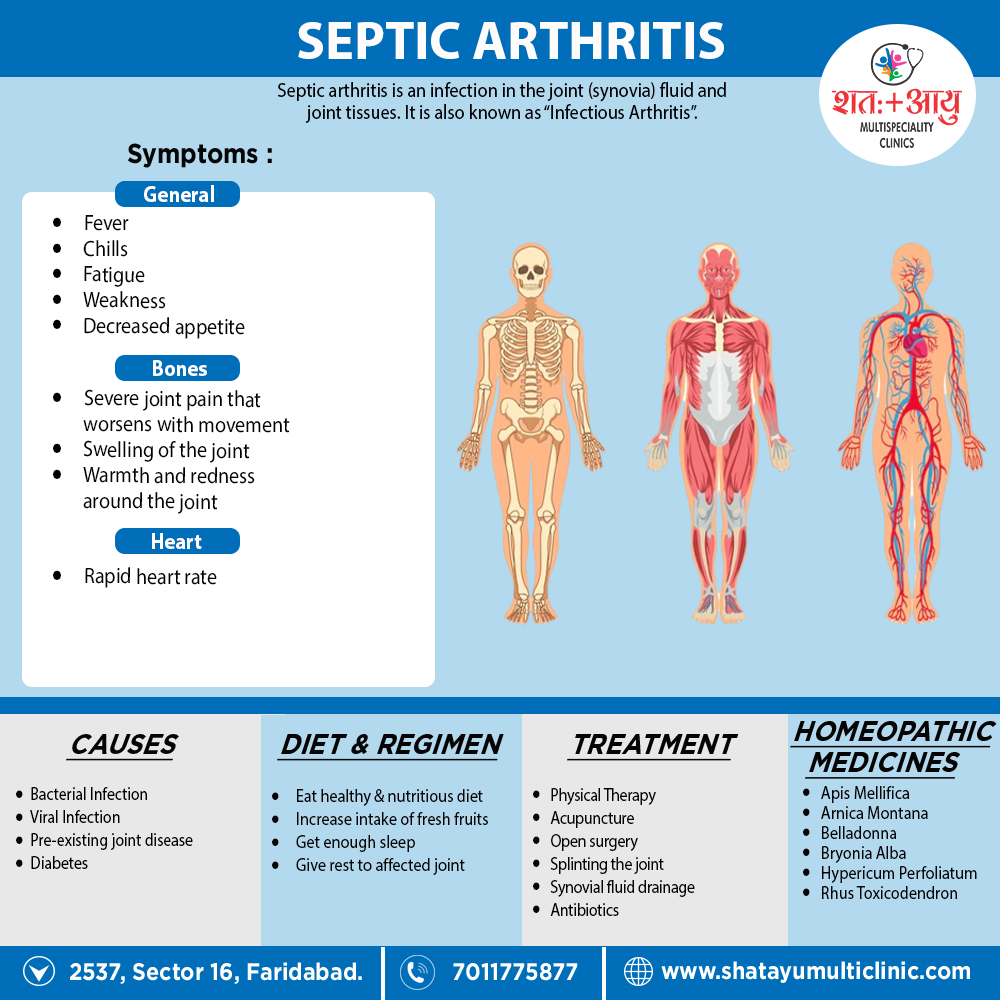
Septic arthritis is the most rapid and destructive joint disease, and is associated with significant morbidity and a mortality of 10%.
This has not improved over the last 20 years, despite advances in antimicrobial therapy.
The incidence is 2–10 per 100,000 in the general population, and 30–70 per 100,000 in those with preexisting joint disease or joint replacement.
Septic arthritis is usually due to haematogenous spread from either skin or upper respiratory tract; infection from direct puncture wounds or secondary to joint aspiration is uncommon.
Risk factors include;
- Increasing age,
- Pre existing joint disease (principally RA),
- Diabetes mellitus,
- Immunosuppression (by drugs or disease),
- Intravenous drug misuse.
In RA, the skin is a frequent portal of entry because of maceration of skin between the toes due to joint deformity and difficulties with foot hygiene due to hand deformity. [1]
Infants and older adults are most likely to develop septic arthritis.
Knees are most commonly affected, but septic arthritis also can affect hips, shoulders and other joints.
The infection can quickly and severely damage the cartilage and bone within the joint, so prompt treatment is crucial. [2]