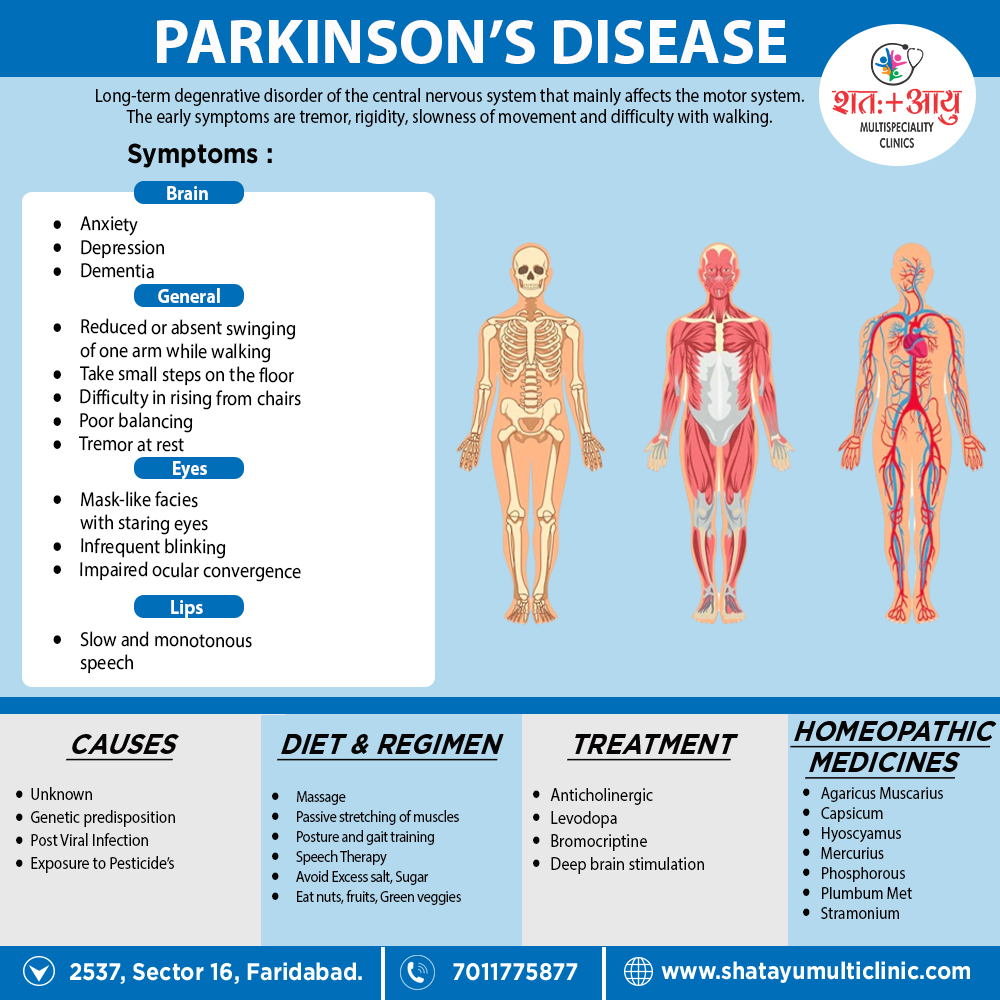
Homeopathic medicines for Parkinson’s disease
Homeopathic medicines are individualized, selected based on the individual case history of the patient, by taking into consideration the cause like hormonal imbalance, nutritional factor, emotional stress, the nature of the patient, and other factors which may be acting as a maintaining cause in the hair loss.
Some of the commonly prescribe remedies are as follows.
AGARICUS MUSCARIS:
This fungus contains several toxic compounds, best known is Muscarin. Agaricus acts as an intoxicant to the brain, producing more vertigo and delirium than alcohol. Jerking twitching trembling and itching are strong indications. Sensation as if pierced. Loquacity, aversion to work, indifference, fearlessness. Weakness in loins. Uncertain gait. Trembling. Trembling. Paralysis of lower limbs, with spasmodic condition of arms.
Worse – open, cold air, especially after eating, after coitus, before a thunder storm. On other hand, Better – moving about slowly.[2]
CAPSICUM:
Manifests its action mainly in chronic rheumatic, arthritic and paralytic affections, indicated by tearing, drawing pains in the muscular and fibrous tissue, with deformities about the joints; progressive loss of muscular strength, tendinous contractors. Heaviness and weakness of extremities Unsteadiness of muscles of forearm and hand. Numbness, loss of sensation in hands. Contracted tendons. Unsteady walking and easy falling. Restless legs at night. Worse – dry, cold winds, specifically, in clear fine weather, motion of carriage. Whereas Better – damp, wet weather, warmth, heat of bed.
HYOSCYAMUS:
Disturbs the nervous system profoundly. It causes a perfect picture of mania of a quarrelsome character. Weakness and nervous agitation. Tremulous weakness and twitching of tendons. In detail, Muscular twitching, spasmodic affections, generally with delirium. Picking at bedclothes, plays with hands. Besides this, Reaches out for things. Spasms also convulsions. Great restlessness; every muscle twitches. Will not be covered. Very suspicious, talkative, obscene, lascivious mania, uncovers body; jealous, foolish. Great hilarity; inclined to laugh at everything. Low, muttering speech.
Worse – night during menses, after eating, when lying down. On the other hand, Better – stooping.
PLUMBUM:
Progressive muscular atrophy. Additionally, Paralysis of single muscles. Locomotor ataxia. Cannot raise or lift anything with the hand. Extension is difficult. Pains in muscles of thighs. Comes in paroxysms. Stinging and tearing in limbs, also twitching and tingling, numbness, pain or tremor. Loss of patellar reflex. Depression. Fear of being assassinated. Quiet melancholy. Slow perception. Loss of memory. Great medicine for PD.
Worse – night, motion. On the other hand, Better – rubbing, hard pressure, physical exertion.[2]
MERCURIUS:
Tremors everywhere. Weakness with ebullitions and trembling from least exertion. Additionally, All memory symptoms are worse at night, from warmth of bed, from damp, cold, rainy weather, worse during perspiration. Complaints increase with sweat and rest; all associated with a great deal of weariness, prostration also trembling. Memory weakened and loss of will-power. Weary of life, mistrustful, thinks he is losing his reason. Weakness of limbs Oily perspiration. Trembling extremities, especially hands. Paralysis agitans.
Worse – night, wet, damp weather, lying on right side, warm room. Better – damp, wet weather, warmth, heat of bed.
PHOSPHORUS:
Irritates, inflames and degenerates mucus membranes also serous membranes, and inflames the spinal cord and nerves. Ascending sensory and motor paralysis from ends of fingers and toes. Weakness also trembling, from every exertion. Can scarcely hold anything with his hands. Arms and legs become numb. Joints suddenly give way. Oversensitive to external impressions – light, sound, odours, electrical changes, thunder storms. Loss of memory. Fidgety.
Worse – twilight, either warm food or drink, lying especially on left side, ascending stairs whereas Better – dark, lying on right side, cold food, open air, cold, sleep.
STRAMONIUM:
The entire force of this drug seems to be expended on the brain. Sensation as if limbs were separated from the body. Delirium tremens. Absence of pain and muscular mobility, especially muscles of expression and locomotion.
Rapid changes from joy to sadness. Convulsions of upper extremities and of isolated groups of muscles. Trembling, twitching of tendons. Besides this, Staggering gait.
Worse – in dark room, when alone, after sleep, on swallowing. On the other hand, Better – from company, warmth.
NOTE ALSO: CAUSTICUM, ALUMINA, AND ZINCUM METALLICUM.[2]