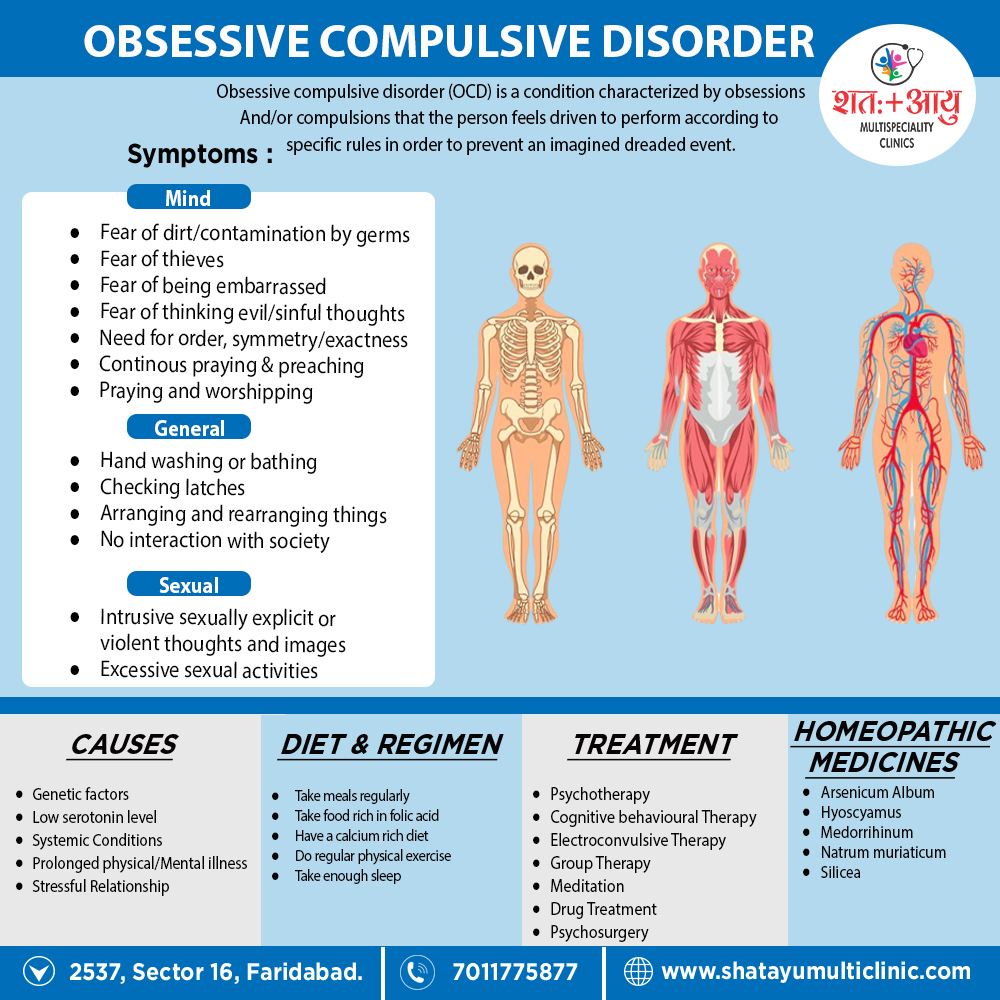
Obsessions are recurrent persistent thoughts, impulses, or images that enter the mind despite efforts to exclude them. The feeling of compelled to undergo the intrusion of a thought, impulse, or image and the resistances produced against them are key characteristics of an obsession. [1]
In India, obsessive compulsive disorder (OCD) is more common in unmarried males, while in other countries, no gender differences are reported.
This disorder is commoner in persons from upper social strata and with high intelligence. The average age of onset is late third decade (i.e. late 20s) in India, while in the Western countries the onset is usually earlier in life.
A summary of long-term follow-up studies shows that about 25% remained unimproved over time, 50% had moderate to marked improvement while 25% had recovered completely. [2]
An obsession is define as:
- An idea, impulse or image which intrudes into the conscious awareness repeatedly.
- It is recognise as one’s own idea, impulse or image but is perceive as ego-alien (foreign to one’s personality).
- It is recognise as irrational and absurd (insight is present).
- Patient tries to resist against it but is unable to.
- Failure to resist, leads to mark distress.
- An obsession is usually associate with compulsion.
A compulsion is define as:
- A form of behaviour which usually follows obsessions.
- It is aim at either preventing or neutralising the distress or fear arising out of obsession.
- The behaviour is not realistic and is either irrational or excessive.
- Insight is present, so the patient realises the irrationality of compulsion.
- The behaviour is perform with a sense of subjective compulsion (urge or impulse to act).
- Compulsions may diminish the anxiety associate with obsessions. [2]