Overview of Mastitis
Risk factors include poor latch, cracked nipples, use of a breast pump, and weaning. [1]
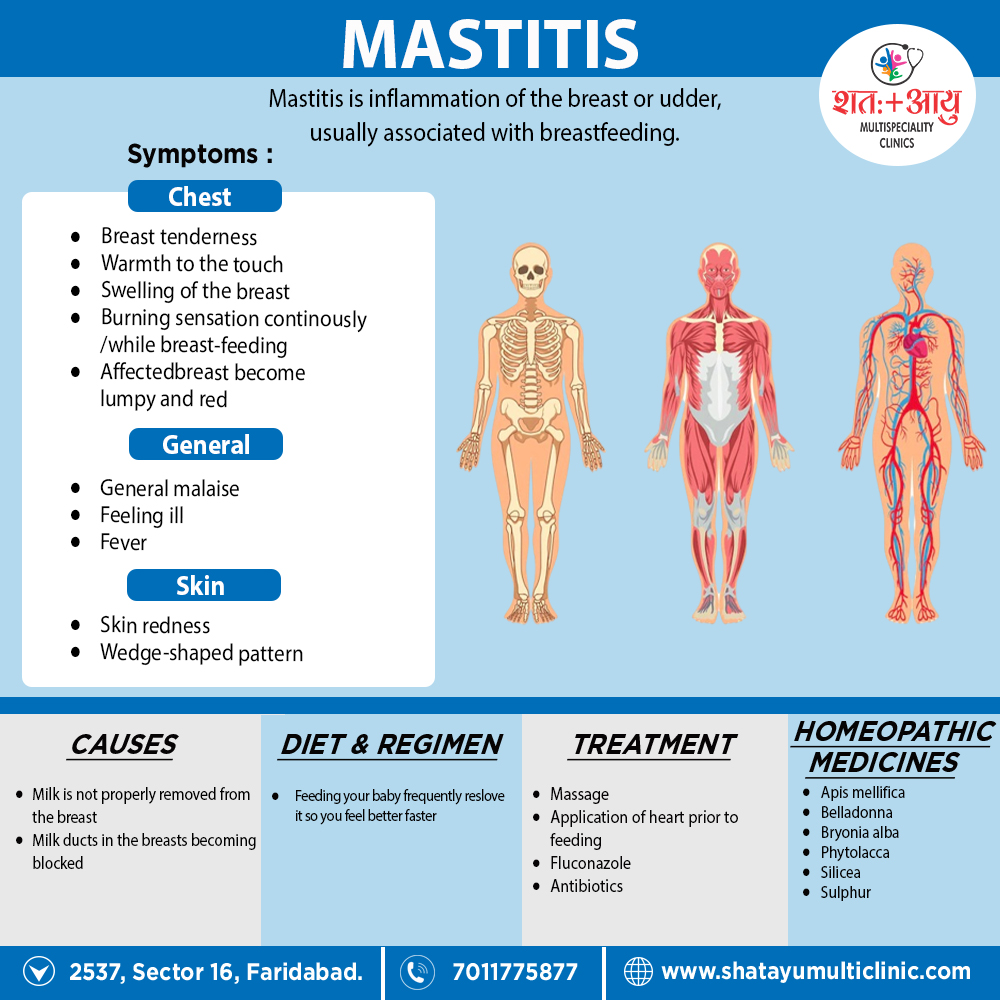
Mastitis is inflammation of the breast or udder, usually associated with breastfeeding.[1]
Risk factors include poor latch, cracked nipples, use of a breast pump, and weaning. [1]
Lactation mastitis usually affects only one breast and the symptoms can develop quickly.
The signs and symptoms usually appear suddenly and they include i.e.:
Some women may also experience flu-like symptoms such as:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Mastitis is inflammation of the breast or udder, usually associated with breastfeeding.
References