Knee pain may result from intraarticular (OA, RA) or periarticular (anserine bursitis, collateral ligament strain) processes or be referred from hip pathology. A careful history should delineate the chronology of the knee complaint and whether there are predisposing conditions, trauma, or medications that might underlie the complaint.
For example, patellofemoral disease (e.g., OA) may cause anterior knee pain that worsens with climbing stairs. [1]
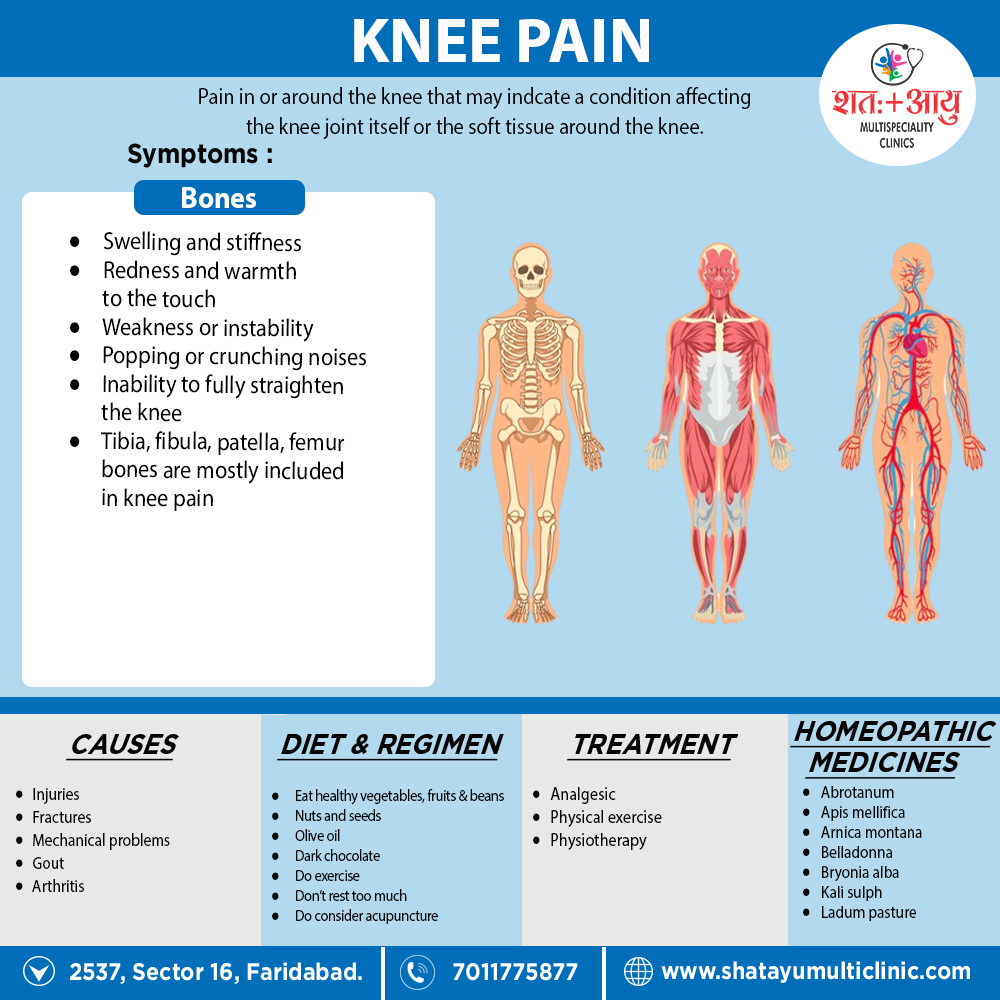
Knee pain can be caused by injuries, mechanical problems, types of arthritis and other problems.
Injuries
A knee injury can affect any of the ligaments, tendons or fluid-filled sacs (bursae) that surround your knee joint as well as the bones, cartilage and ligaments that form the joint itself. Some of the more common knee injuries include:
ACL injury
An ACL injury is a tear of the anterior cruciate ligament (ACL). An ACL injury is particularly common in people who play basketball, soccer or other sports that require sudden changes in direction. [2]
Fracture
The bones of the knee, including the kneecap (patella), can be broken during falls or auto accidents. Also, people whose bones have been weakened by osteoporosis can sometimes sustain a knee fracture simply by stepping wrong.
Torn meniscus
The meniscus is the tough, rubbery cartilage that acts as a shock absorber between your shinbone and thighbone. It can be torn if you suddenly twist your knee while bearing weight on it.
Knee bursitis
Some knee injuries cause inflammation in the bursae, the small sacs of fluid that cushion the outside of your knee joint so that tendons and ligaments glide smoothly over the joint.
Patellar tendinitis
Tendinitis causes irritation and inflammation of one or more tendons — the thick, fibrous tissues that attach muscles to bones. This inflammation can happen when there’s an injury to the patellar tendon, which runs from the kneecap (patella) to the shinbone and allows you to kick, run and jump. Runners, skiers, cyclists, and those involved in jumping sports and activities may develop patellar tendinitis.[2]
Mechanical problems
Some examples of mechanical problems that can cause knee pain include:
Loose body-
Sometimes injury or degeneration of bone or cartilage can cause a piece of bone or cartilage to break off and float in the joint space. This may not create any problems unless the loose body interferes with knee joint movement, in which case the effect is something like a pencil caught in a door hinge.
Iliotibial band syndrome-
This occurs when the tough band of tissue that extends from the outside of your hip to the outside of your knee (iliotibial band) becomes so tight that it rubs against the outer portion of your thighbone. Distance runners and cyclists are especially susceptible to iliotibial band syndrome.
Dislocated kneecap-
This occurs when the triangular bone that covers the front of your knee (patella) slips out of place, usually to the outside of your knee. In some cases, the kneecap may stay displaced and you’ll be able to see the dislocation.
Hip or foot pain-
If you have hip or foot pain, you may change the way you walk to spare your painful joint. But this altered gait can place more stress on your knee joint and cause knee pain.
Arthritis
The varieties most likely to affect the knee include:
- Sometimes called degenerative arthritis, osteoarthritis is the most common type of arthritis. It’s a wear-and-tear condition that occurs when the cartilage in your knee deteriorates with use and age.
Rheumatoid arthritis-
The most debilitating form of arthritis, rheumatoid arthritis is an autoimmune condition that can affect almost any joint in your body, including your knees. Although rheumatoid arthritis is a chronic disease, it tends to vary in severity and may even come and go.
- This type of arthritis occurs when uric acid crystals build up in the joint. While gout most commonly affects the big toe, it can also occur in the knee.
- Often mistaken for gout, pseudogout is caused by calcium-containing crystals that develop in the joint fluid. Knees are the most common joint affected by pseudogout.
Septic arthritis-
Sometimes your knee joint can become infected, leading to swelling, pain and redness. Septic arthritis often occurs with a fever, and there’s usually no trauma before the onset of pain. Septic arthritis can quickly cause extensive damage to the knee cartilage. If you have knee pain with any of the symptoms of septic arthritis, see your doctor right away.[2]
Other problems
Patellofemoral pain syndrome
Patellofemoral pain syndrome is a general term that refers to pain arising between the kneecap and the underlying thighbone. It’s common in athletes; in young adults, especially those whose kneecap doesn’t track properly in its groove; and in older adults, who usually develop the condition as a result of arthritis of the kneecap. [2]
Patellofemoral disease
Patellofemoral disease (e.g., OA) may cause anterior knee pain that worsens with climbing stairs. The knee should be carefully inspected in the upright (weight-bearing) and supine positions for swelling, erythema, malalignment, visible trauma, muscle wasting, and leg length discrepancy. The most common malalignment in the knee is genu varum (bowlegs) or genu valgum (knock-knees) resulting from asymmetric cartilage loss medially or laterally. [1]
Bony swelling of the knee joint
Bony swelling of the knee joint commonly results from hypertrophic osseous changes seen with disorders such as OA and neuropathic arthropathy. Swelling caused by hypertrophy of the synovial or synovial effusion may manifest as a fluctuant, ballotable, or soft tissue enlargement in the Bicipital tendon Humours Glenohumeral (shoulder) joint Subscapularis muscle suprapatellar pouch (suprapatellar reflection of the synovial cavity) or regions lateral and medial to the patella. [1]
Application of manual pressure lateral to the patella may cause an observable shift in synovial fluid (bulge) to the medial aspect. The examiner should note that this manoeuvre is only effective in detecting small to moderate effusions (<100 mL). Inflammatory disorders such as RA, gout, pseudogout, and psoriatic arthritis may involve the knee joint and produce significant pain, stiffness, swelling or warmth. Additionally, a popliteal or Baker’s cyst may be palpated with the knee partially flexed and is best viewed posteriorly with the patient standing and knees fully extended to visualize isolated or unilateral popliteal swelling or fullness. [1]