Overview of Hepatitis A
Hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV), the HBV-associated delta agent or hepatitis D virus (HDV), and hepatitis E virus (HEV). All these human hepatitis viruses are RNA viruses, except for hepatitis B, which is a DNA virus but replicates like a retrovirus.
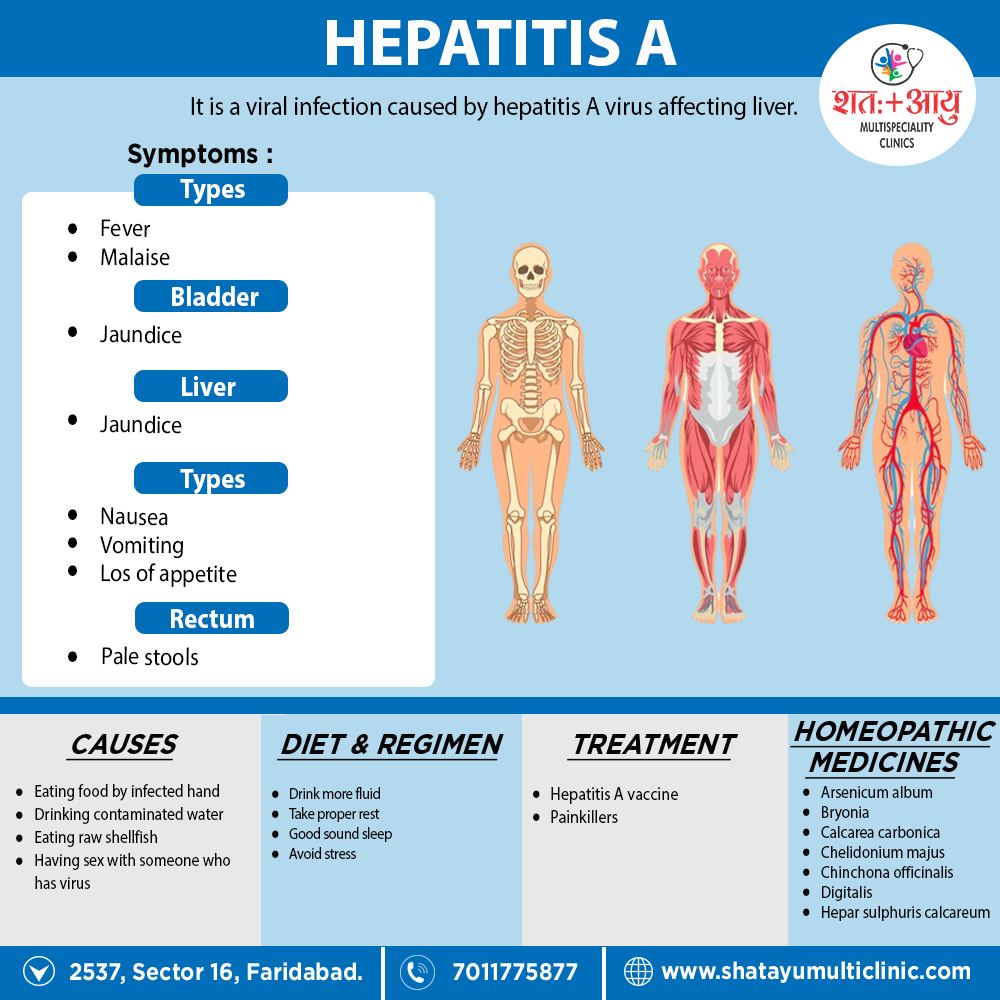
Although these agents can be distinguished by their molecular and antigenic properties, all types of viral hepatitis produce clinically similar illnesses. These range from asymptomatic and inapparent to fulminant and fatal acute infections common to all types, on the one hand, and from subclinical persistent infections to rapidly progressive chronic liver disease with cirrhosis and even hepatocellular carcinoma, common to the bloodborne types (HBV, HCV, also HDV), on the other. [2]
Acute viral hepatitis may be asymptomatic, marked only by an increase in aminotransferase levels, or symptomatic with or without jaundice or sub fulminant or fulminant depending on the causative agent.
Though the natural history of acute hepatitis can vary according to the etiological agent, it can be divided as follows depending on clinical features and laboratory findings:
-
Prodromal period
- Bilirubinuria appears earlier than a rise in serum bilirubin.
- Serological viral markers help in arriving at a diagnosis.
- Urobilinogen and total bilirubin rise occur before clinical jaundice.
- Liver enzymes AST and ALT are > 500 units
- Leucopaenia may be observed with onset of fever.
-
Acute icteric stage
- Bilirubin rises, plateaus and then gradually decreases.
- Serum AST and ALT rise and fall rapidly and reach normal range in 2 to 5 weeks.
- ESR is raised initially and falls during convalescence
-
Defervescent stage
- Diuresis occurs at onset of convalescence.
- Bilirubinuria disappears, serum bilirubin is still increased.
- Urine urobilinogen increases.
- bilirubin becomes normal after 3 to 6 weeks [1]