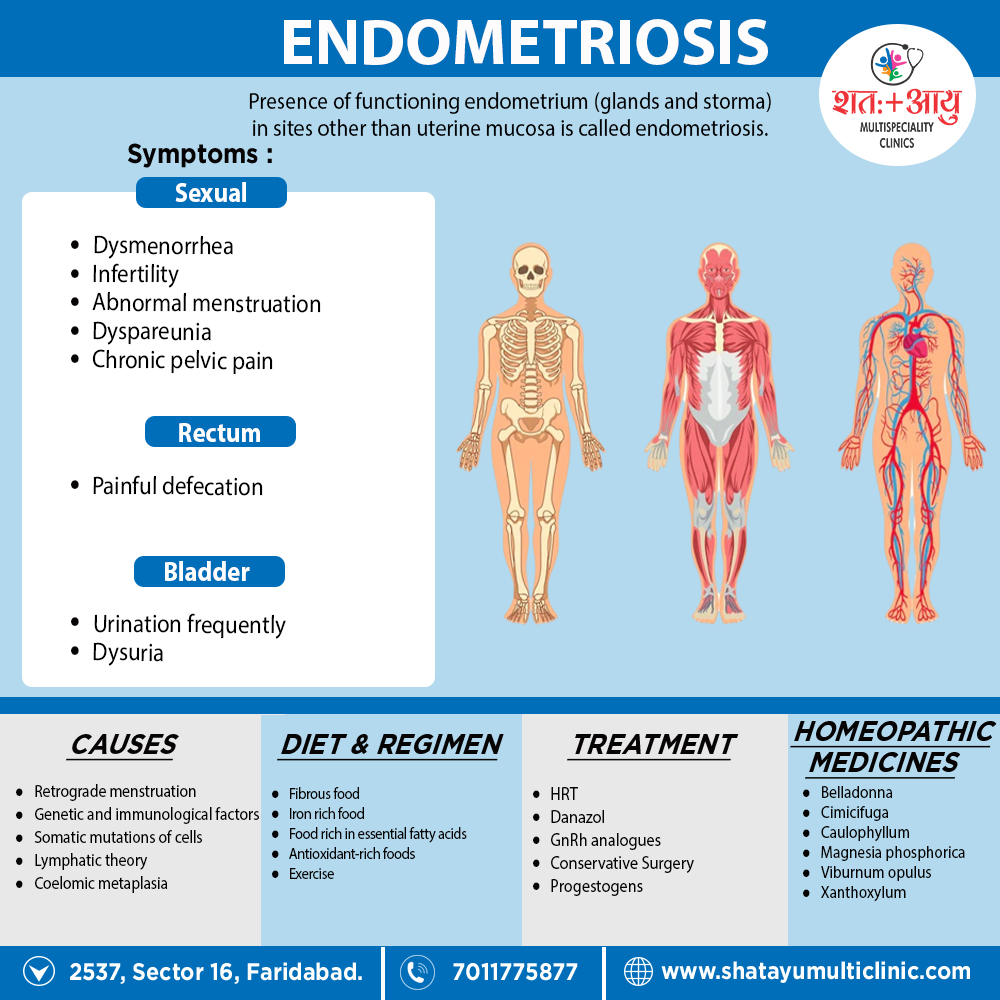
Homeopathic treatment base on individualization in which a doctor selects a medicine according to your/ patients constitution rather than matching only symptoms similarity, so before taking any homoeopathic medicine you have to firstly consult a homoeopathic physician for your concern problem’s, there are so many remedies are useful for this condition but some few therapeutic indications of homeopathic remedies in the cases of Endometriosis are as below.
| Cimicifuga. [Cimic] |
| The characteristic indication for this remedy in dysmenorrhea is pain flying across the pelvic region from one side to the other. It is especially useful in rheumatic and neuralgic cases, and in congestive cases it may also be thought of along with Belladonna and Veratrum viride. Headache preceding menses; during menses sharp pains across abdomen, has to double up, labor-like pains, and during menstrual interval debility and perhaps a scanty flow. The resin Macrotin is preferred by many practitioners. The pains of Cimicifuga are not severe and intense nor felt with such acuteness as are those of Chamomilla. [2] |
Caulophyllum. [Caul]
The dysmenorrhea of Caulophyllum is essentially spasmodic in character; the pains are bearing down in character. It produces a continued spasm of the uterus simulating first stage of labor; the flow is mostly normal in quantity. The spasmodic intermittent pains which call for Caulophyllum are in the groins, a useful remedy in these spasmodic cases if given between the periods. to various part of the body.
Magnesia muriatic is also a remedy which may be studied in uterine spasm. Gelsemium is similar in many respects to Caulophyllum. It is very useful remedy in neuralgic and congestive dysmenorrhea when there is such bearing down. The pains are spasmodic and labor-like, with passages of large quantities of pale urine. It is one of the best given low in hot water. It will surely relieve the pains at the start.
Belladonna. [Bell]
The congestive forms of dysmenorrhea would call for Belladonna. There is pain preceding the flow and a sensation of heaviness as if everything would protrude from the vulva, relieved by sitting up straight. The pains come on suddenly and cease suddenly; the flow is offensive and clotted. The dysmenorrhea is intensely painful, the vagina is hot and dry and the pains are cutting through the pelvis in a horizontal direction, not around the body, as in Platinum and Sepia.
Veratrum viride is use with benefit in congestive dysmenorrhea, in plethoric women, accompany with strangury and preceded by intense cerebral congestion, also spasmodic dysmenorrhea at or near the climacteric. These are conditions in which the old school knows only Opium, yet these remedies are far superior to that drug, often curing permanently while Opium is only palliative.[2]
Viburnum opulus. [Vib]
This remedy produces a sudden pain in the region of the uterus before menstruation and much backache during menses. In neuralgic and spasmodic dysmenorrhea, it has achieved considerable reputation. Dr. Hale considers it specific in this form of painful menstruation. Its chief indications seem to be in the character of the pains, which are spasmodic. Spasmodic dysuria in hysterical subjects also calls for Viburnum.
Its keynotes, therefore, are bearing down, aching in sacral and pubic region, excruciating, cramp, colicky pains in hypogastrium, much nervousness, and occasional shooting pains in the ovaries. Like Sepia, Viburnum has pains going around the pelvis and also the empty, gone feeling in the stomach; but the bearing down is more violent, culminating in an intense uterine cramp. More indicated by clinical experience than by its pathogenesis.[2]
Xanthoxylum. [Xanth]
This remedy has about only one use in homoeopathic medicine, and that is in dysmenorrhea and uterine pains. It is useful where the pains are agonizing, burning, extending down thighs along the crural nerves with a feeling as if the limbs is paralyze, the menstruation is usually profuse and with it agonizing bearing down pains; chiefly left sided are the pains of Xanthoxylum, though it also affects the right ovary.
It corresponds closely to the neuralgic form of dysmenorrhea. Hale says that the neuralgic element must predominate to have the remedy efficacious. Some further symptoms may be headache over the left eye the day before the menses, and it seems to correspond to women of spare habits and of a delicate, nervous temperament.[2]
Magnesia Phosphorica. [Mag-p]
Perhaps no remedy has achieved a greater clinical reputation in dysmenorrhea than has Magnesia Phosphorica. The pains calling for it are neuralgic and crampy preceding the flow, and the great indication for the use of this remedy is the relief from warmth and the aggravation from motion. In neuralgia of the uterus Magnesia Phosphorica vies with Cimicifuga. Uterine engorgements with the characteristic crampy pains will indicate the remedy. It has also been used successfully in membranous dysmenorrhea. We have very few remedies for this affection.
Borax is one, but it is often unsuccessful, there seems to be no very special characteristic for it, unless it be the fear of downward motion which might exist in some cases. Hale mentions Viburnum, Guaiacum and Ustilago, besides Borax, for membranous dysmenorrhea. Their indications are chiefly empirical. Colocynth, a useful remedy in dysmenorrhea, may be compared with Magnesia Phosphorica. The symptoms of Colocynth are severe left-sided ovarian pains, causing patient to double up; pains extend from umbilicus to genitals.[2]
Pulsatilla. [Puls]
Dysmenorrhea calls for Pulsatilla when the menses are dark in color and delayed; the flow will be fitful and the more severe the pains are the chillier the patient will get. The pains gripe and double the patient up. It is perhaps more useful when give between the periods, and in congestive dysmenorrhea, from wetting of the feet, it is compared with Aconite, but in Aconite the discharge is bright red instead of dark.
Chamomilla and Cocculus are two remedies which run along side by side with Pulsatilla in dysmenorrhea, and all need careful individualization. Chamomilla has also a dark flow, but it has such characteristic mental symptoms of crossness and incivility that it cannot be mistaken. It will relieve many cases (12X). Cocculus also has dark flow. It has a pain as if sharp stones were rubbing against each other in the abdomen from accumulation of flatus; the pains are worse at night, awaken the the patient and make her irritable. Menses come too early, sometimes nausea is an accompaniment. It also is said to be more efficacious given between the periods. The mental condition of Pulsatilla, if present, will always indicate the remedy. Further, if the pains shift about the indications of Pulsatilla are still stronger.[2]
Cocculus. [Cocc]
A most useful remedy in dysmenorrhea and scanty, irregular menstruation. Uterine cramps. Profuse discharge of clotted blood and severe headache accompanied by nausea; a heaving up and down of the stomach as in seasickness. It suits cases on the borderland between the neuralgic and congestive types of dysmenorrhea. Uterine cramps with suppressed irregular menstruation and a sero-purulent bloody discharge were favorite indications of Dr. Conrad Wesselhoeft. Gelsemium IX has also proved useful in the spasmodic form. Ignatia has dysmenorrhea with menstrual colic or bearing-down in the hypogastric region, hysterical labor-like pains relieved by pressure.[2]