Homeopathic medicines are individualized, selected based on the individual case history of the patient, by taking into consideration the cause like hormonal imbalance, nutritional factor, emotional stress, the nature of the patient, and other factors which may be acting as a maintaining cause in the diphtheria.
Diphtheria, as it is an acute problem, requires a constitutional treatment. Homeopathy focuses on the root cause of the problem and helps in the treatment of diphtheria.
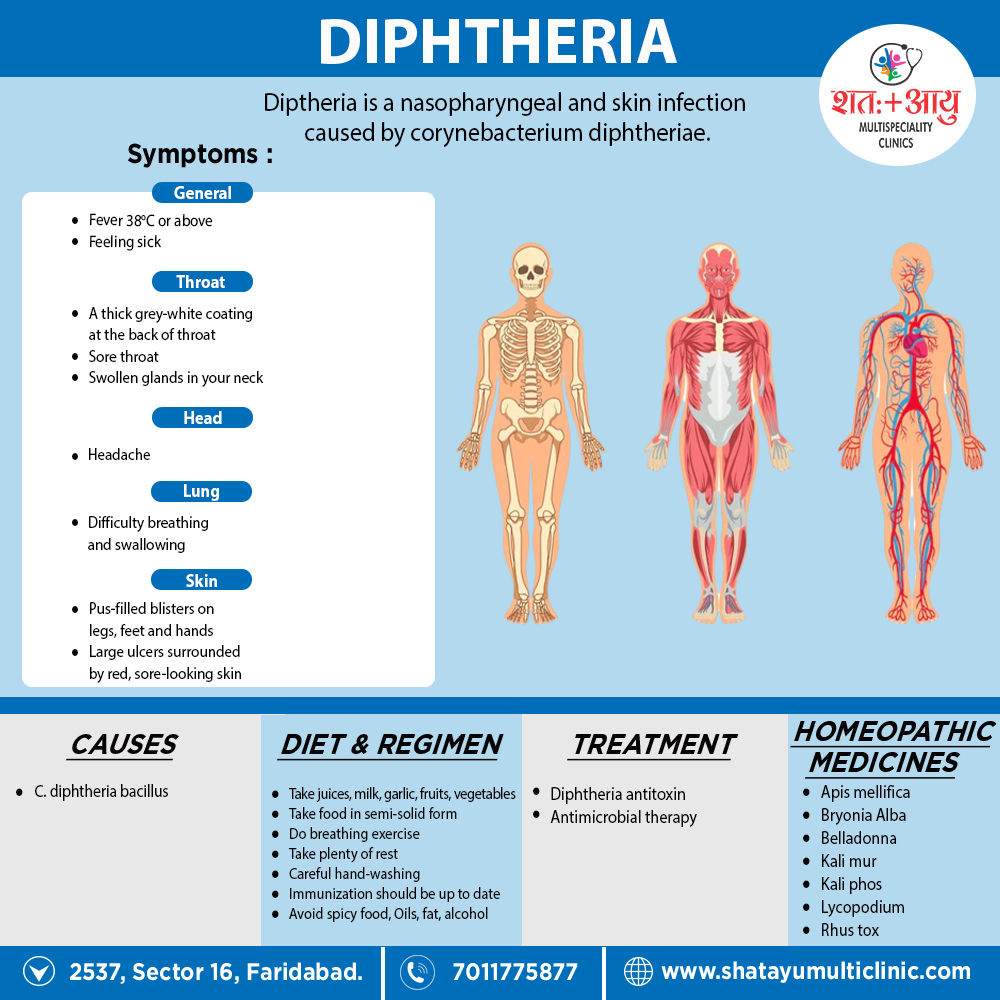
Medicines:
-
Bryonia Alba:
Great prostration; patient cannot bear to be moved; complains of pains everywhere when moved; white tongue; dry mouth; thirst for large quantities of water.
-
Belladona:
Restless; complains of sore throat, which looks highly inflamed; pupils large; drowsy, but unable to sleep; starts suddenly out of sleep
-
Lycopodium:
Throat brownish red; worse right side; worse from swallowing warm drinks; nose stopped up. Furthermore; patient cannot breathe with mouth shut; keeps mouth constantly open, slightly protruding the tongue, which gives a silly expression; unsteady step; on awaking from short nap he is cross; kicks; is naughty (if a child); or jumps up in bed, stares about, also knows nobody seemingly dreaming with open eyes; frequent jerkings of lower limbs, mostly with a groan, awake or slumbering; great fear of being left alone.
- Rhus
tox:
Restless; wants to be carried about; wakes complaining of pain in throat; bloody saliva runs out of mouth during sleep; parotid glands good deal swollen; transparent jelly-like discharges form bowels at stool or afterwards
-
Apis mellifica:
Great debility from the beginning; membranes at once assume dirty greyish colour, or there is great oedema of soft palate and much puffiness round the eyes; pain in ears on swallowing; an itching, stinging eruption on skin; sensation of weakness in larynx; numbness of feet and hands and even paralysis. (Apis is incompatible with Rhus, and should not be given immediately after it or Rhus after Apis.)
- Kali Mur: For typical diphtheria.
- Kali phos:
When the breath becomes putrid and the throat gangrenous or the case paralytic.
-
Ammonium carb:
Diphtheria of scrofulous persons with swelling of the glands of the neck; putrid sore throat, burning pain with roughness also scraping in throat; tendency to gangrene in throat. Additionally, nose obstructed, child aroused from sleep by want of breath; great prostration; excessive sensitiveness to cold air and cold drinks; Besides this; cerebral symptoms
-
Arsenicum iod:
Diphtheritic croup, deposit covering mouth from fauces to outer edge of lips and external auditory canal; foul breath; short, difficult respiration and symptoms of adynamia marked enlargement of lymphatic glands, WEAK HEART.
10. Bromium:
Malignant forms of diphtheria, invading LARYNX DOWN RESPIRATORY ORGANS, leaving great weakness and lassitude; no fever, cool skin, sweating and spasm; husky tone of voice, rattling of mucus in larynx when coughing , cough has a croupy sound, with strangling of mucus in larynx when coughing rattling mucus in breathing; face ashy-gray, cheeks sunken, stiffness of neck, prostration Suits children with fair hair and skin, blue eyes, etc., also Teste affirms that milk neutralizes the action of Brom. And Iod. (Kali bi. no spasm). [4]