Overview of Cataract
Most cataracts develop slowly as a result of aging, leading to gradual impairment of vision.
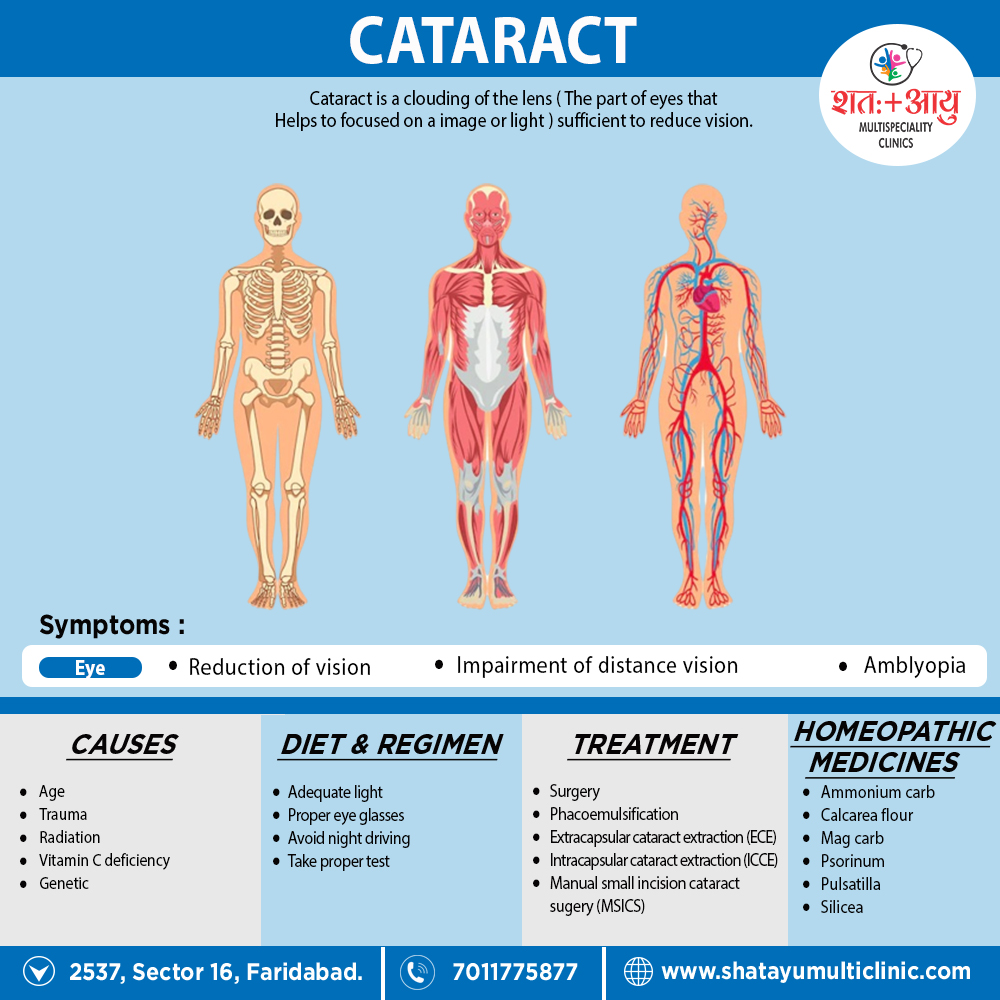
Cataract is a clouding of the lens (The part of eyes that Helps to focused on an image or light) sufficient to reduce vision.[1]
Most cataracts develop slowly as a result of aging, leading to gradual impairment of vision.
Accumulation of clumps of protein or yellow-brown pigment in the lens that reduces transmission of light to the retina at the back of the eye.[1]
Cataracts acquired in a variety of genetic diseases, such as Myotonic dystrophy, neurofibromatosis type 2, and galactosemia.[1]
Cataract can detected by noting an impaired red reflex when viewing light reflected from the fundus with an ophthalmoscope or by examining the dilated eye with the slit lamp.[1]
The only treatment for cataract surgical extraction of the opacified lens. Millions of cataract operations performed each year around the globe. The operation generally done under local anesthesia on an outpatient basis.
A plastic or silicone intraocular lens placed within the empty lens capsule in the posterior chamber, substituting for the natural lens and leading to rapid recovery of sight. More than 95% of patients who undergo cataract extraction can expect an improvement in vision.
In some patients, the lens capsule remaining in the eye after cataract extraction eventually turns cloudy, causing secondary loss of vision. A small opening, called a posterior capsulotomy, made in the lens capsule with a laser to restore clarity.[1]
Cataracts may be
The main types of age-related cataracts are nuclear sclerosis, cortical, and posterior subcapsular.
Cataracts can be classified by using the lens opacities classification system LOCS III. In this system, cataracts are classified based on type as
To determine whether you have a cataract, your doctor will review your medical history and symptoms, and perform an eye examination. Your doctor may conduct several tests, including:
A visual acuity test uses an eye chart to measure how well you can read a series of letters. Your eyes are tested one at a time, while the other eye is covered. Using a chart or a viewing device with progressively smaller letters, your eye doctor determines if you have 20/20 vision or if your vision shows signs of impairment.
A slit lamp allows your eye doctor to see the structures at the front of your eye under magnification. The microscope is called a slit lamp because it uses an intense line of light, a slit, to illuminate your cornea, iris, lens, and the space between your iris and cornea. The slit allows your doctor to view these structures in small sections, which makes it easier to detect any tiny abnormalities.
To prepare for a retinal exam, your eye doctor puts drops in your eyes to open your pupils wide (dilate). This makes it easier to examine the back of your eyes (especially retina). Using a slit lamp or a special device called an ophthalmoscope, your eye doctor can examine your lens for signs of a cataract.
This test measures fluid pressure in your eye. There are multiple different devices available to do this.[5]
These complications i.e.
Risk factors such as UVB exposure and smoking can addressed.
Although no means of preventing cataracts has been scientifically proven, wearing sunglasses that counteract ultraviolet light may slow their development.
While adequate intake of antioxidants (such as vitamins A, C, and E) has thought to protect against the risk of cataracts, clinical trials have shown no benefit from supplements; though evidence mixed, but weakly positive, for a potential protective effect of the nutrient’s lutein and zeaxanthin.[2]
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Cataract is a clouding of the lens (The part of eyes that Helps to focused on an image or light) sufficient to reduce vision.
References: