Cannabis Use Disorder:
Cannabis produces more than 400 identifiable chemicals of which about 50 are cannabinoids, the most active being Δ-9- tetrahydrocannabinol (Δ9THC). The pistillate form of the female plant is more important in cannabis production.
Recently, a Gi-protein (in other words, inhibitory G-protein) linked cannabinoid receptor has found (especially, in basal ganglia, hippocampus and cerebellum) which inhibits the adenylate cyclase activity in a dose-dependent manner.
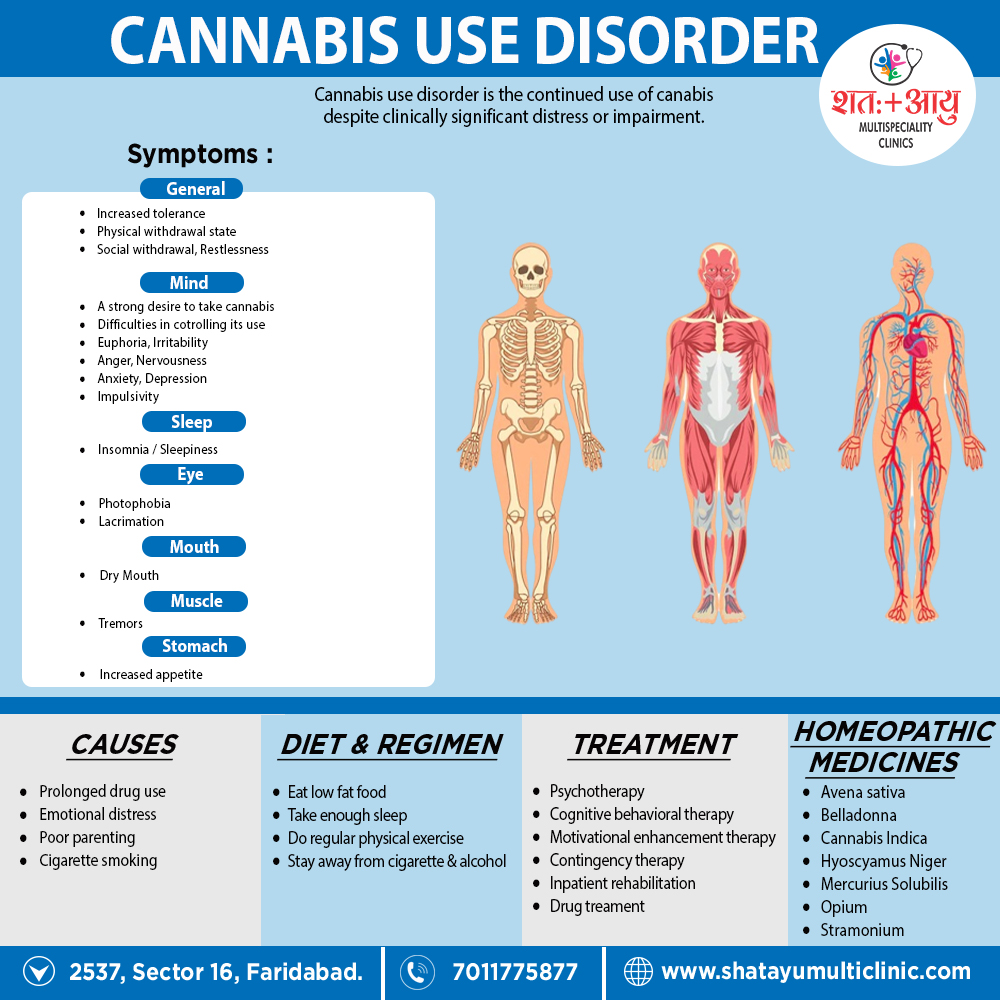
Cannabis produces a very mild physical dependence, with a relatively mild withdrawal syndrome, i.e.
- Fine tremors
- Irritability
- Restlessness
- Nervousness
- Insomnia
- Decreased appetite also craving
In detail, this syndrome begins within few hours of stopping cannabis use also lasts for 4 to 5 days. However, some health professionals feel that there is no true physical dependence with cannabis.
On the other hand, psychological dependence ranges from mild (in other words, occasional ‘trips’) to marked (e.g. compulsive use). Furthermore, All the active ingredients called as marijuana or marihuana.
It can detected in urine for up to 3 weeks after chronic heavy use.