Homeopathic Treatment of Atrophic Rhinitis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
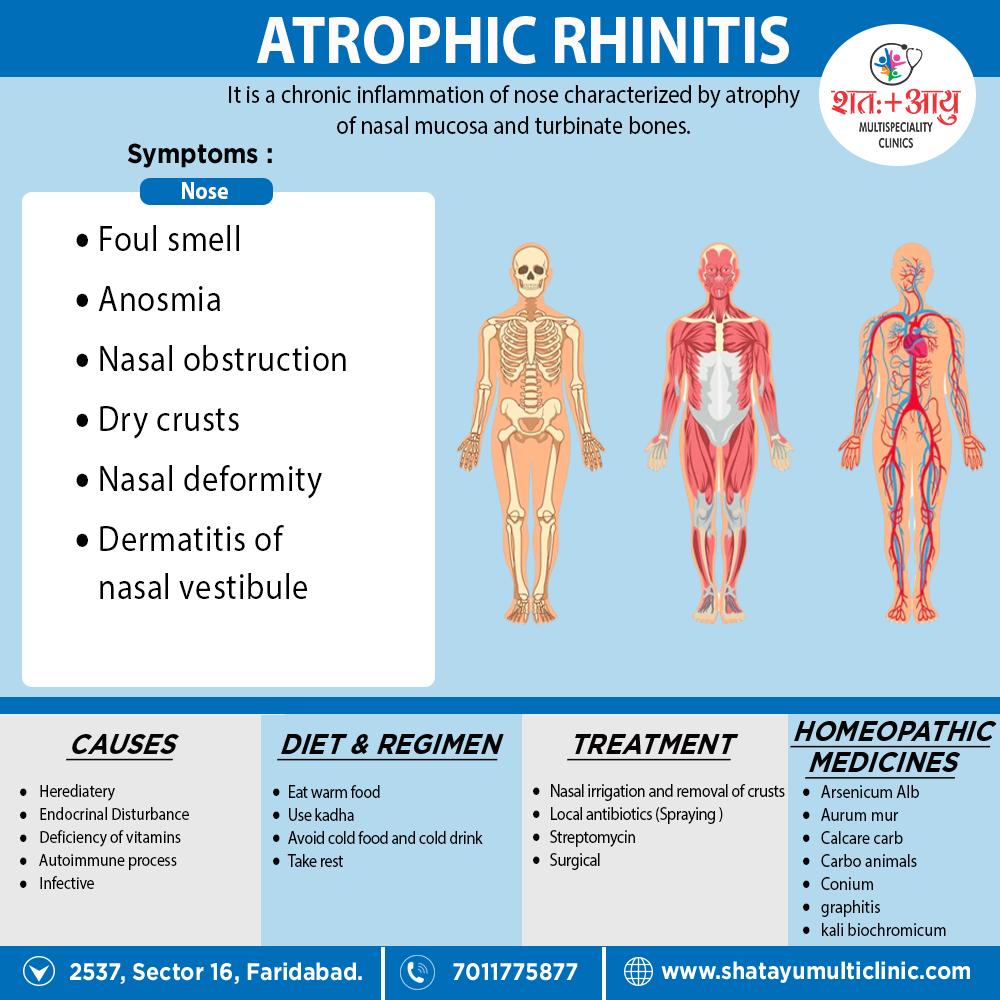
Homeopathic Medicines for Atrophic Rhinitis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Alumen
Lupus, cancer, polypi of nose, sanious discharge, especially when ulceration is present.
Alumina
Soreness and scabs nose discharge of thick, yellow mucous or of dry, hard, yellow-green plugs; the parts, especially septum narium, swollen, red and sore to touch,
(<) evenings; point of nose cracked; WEAK OR ENTIRE LOSS OF SMELL.
Arsenicum Album
Indicated especially in Rhinitis. Cancer, ulcer on right alae nasi, burning, stinging, painful, forming a thick, hard crust, which comes off and leaves a bleeding, mattery surface soon followed by another crust; nostrils; corners of mouth also anus red and excoriated; CANNOT BREATHE THROUGH NOSTRILS WHEN ASLEEP; nose swollen, burns,
coppery-red, with desire for liquors; ichorous, sanious and foetid discharges, with marked prostration and great general debility (Ars. iod.).[2]
Asafoetida
Offensive, greenish discharge from nose, with caries of bones and a feeling as if nose would burst; numbness of bones of face; pimple on tip of nose; small tubercles on cheeks; TEARING PAINS FROM WITHIN OUTWARD in bones of nose, (<) at night. Mercurio- syphilis and scrofula
Aurum Met
Scrofulous and syphilitic affections of bones of nose and face; caries of bones of nose and palate; PUTRID SMELL WHEN BLOWING NOSE, RECOGNIZE BY PATIENT, though olfaction impair; excessively foetid discharge; burning, itching, smarting soreness in nose which is sensitive to touch; unbearable frontal headache; caries extends into cheek-bones, with same tearing, boring pain; bony destruction of ear with Obstinate Otorrhea: Yellow, Thick discharge from nose, or dry firm pieces are blowing out, always of an offensive odor: nose sunken in, perforation of septum.
Aurum Mur
Specifically indicated medicine for Rhinitis Ozaena scrofulous with unbearable odor: Nasal cavity ulcerated deep in, with dry yellowish scruff and senses of obstruction; nostrils stuffed up with hard crusts; lupus of alae nasi, ulceration of soft parts with perforation of Septum
Calcarea Carb
Swelling of nose and upper lip in children, with acrid discharge; purulent, thick, or yellow-red discharge, making lip sore; specifically red itching pustules on upper lip and cheeks; nose swollen inside and outside; impaired smell.; Additionally, EPISTAXIS FREQUENT AND PROFUSE, ALMOST TO FAINTING; loud breathing through nose.
Calcarea Flour
Copious, offensive, thick, greenish-yellow discharge with OSSEOUS GROWTHS IN NOSE; Moreover, blowing of much mucus from nose with ineffectual desire to sneeze.[2]
Carbo animalis
Scrofulous ozaena; swelling of nose, with pimples inside and outside, forming crusts which last a long time; vesicle at right nostril with malignant ulcerations; LITTLE BOILS INSIDE OF NOSE, WITH TENSE ALSO BURNING SENSATION, (<) during menses; saddle across nose with copper-colored eruption. Lastly, Carcinoma nasi.
Conium maculatum
Ozaena with burning in nostrils and stitching pain in septum; discharge of pus and blood from nose; additionally, boring in nostrils; smell of animals in back part of nose; fibrous polypi, hard and elastic, pricking also itching after touching or handling; EXCESSIVELY ACUTE SMELL, WITH PURULENT DISCHARGE.
Elaps cor
Offensive discharge from nose also throat, smelling like putrid herring pickle; posterior wall of throat covered with a dry greenish-yellow scab, Furthermore, extending up to nose; pains from root of nose to ears when swallowing; sense of smell; gone; NOSE BLEEDS WHEN VIOLENTLY BLOWN.
Graphitis
Indicated especially in Rhinitis. Dry scabs in nose, with sore, cracked and ulcerated nostrils; frequently discharge of thick, yellowish, fetid mucus from nose, which may form either hard masses or crusts; loss of smell dryness of noise; Besides this, discharge from nose MUCH MORE FOETID DURING MENSES, catches cold easily; oozing behind ears.[2]
Kali Brom
NOSE FEELS UNNATURALLY DRY, Moreover, being obstruct by large clinkers of dark-greenish, fetid, hard masses, hawk up from post- nasal space, (<) morning till noon; rapid exfoliation also ulceration; loss of smell; PERFORATING ULCERS ON SEPTUM AND ELSEWHERE; desires also fulness from inflammation of frontal sinuses; ropy, tough mucous discharge from posterior nares, offensive or not; polypus nasi.
Mercurious Cor
Ozaena, discharge from nose like glue, drying up in posterior nares; perspiration of septum; NOSE STOPPED UP AND RUNS AT THE SAME TIME; rawness and smarting in nostrils.
Mercurious Iod flavus
Septum sore with sharp pain; much mucus descends into throat, causing hawking; constant inclination to swallow; thick yellow coating on back of tongue.
Nitric Acid
Mercurio-syphilis; foetid, yellow, corroding nasal discharge; generally, ozaena with ulcers; STITCHES IN NOSE AS FROM SPLINTERS; dirty, bloody mucus from posterior nares; large, soft protuberances on alae, covered with crusts; green casts from nose every morning.[2]
Peru Balsam
Ozaena with ulceration; discharge also thick.
Sepia
Ozaena scrofulosa, catches cold easily from deficiency of vital heat; loss of smell or foetid smell before nose; blowing of large lumps of yellow-green mucus or crusts with blood from nose; painful eruption on tip of nose; goneness in epigastrium; sweat in axillae, palms of hands and soles of feet.
Silicea
Gnawing and ulcers high up the nose, with great sensitiveness of place of contact nose inwardly dry, excoriated, covered with crusts; obstructed mornings, fluent during day; intolerable itching of tip of nose; cold nose
Therideone
Chronic catarrh, discharge offensive-smelling, thick, yellow or yellowish-green; caries of nasal bones; dull, thick, heavy sensation in forehead or throbbing extending to occiput; trickling into pharynx; itching behind ears, she would like to scratch them off.
Thuja
SMELL IN NOSE AS OF FISH BRINE; painful scabs in nostrils; blows out much thick green mucus mixed with blood and pus; later brown scabs from; nose sore; red eruption on alae, often moist; skin of face greasy; watery, purulent otorrhea, smelling like putrid meat (Tell. like fish brine); persistent insomnia; sycosis [2]