Homeopathic Treatment of Alzheimer’s Disease
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
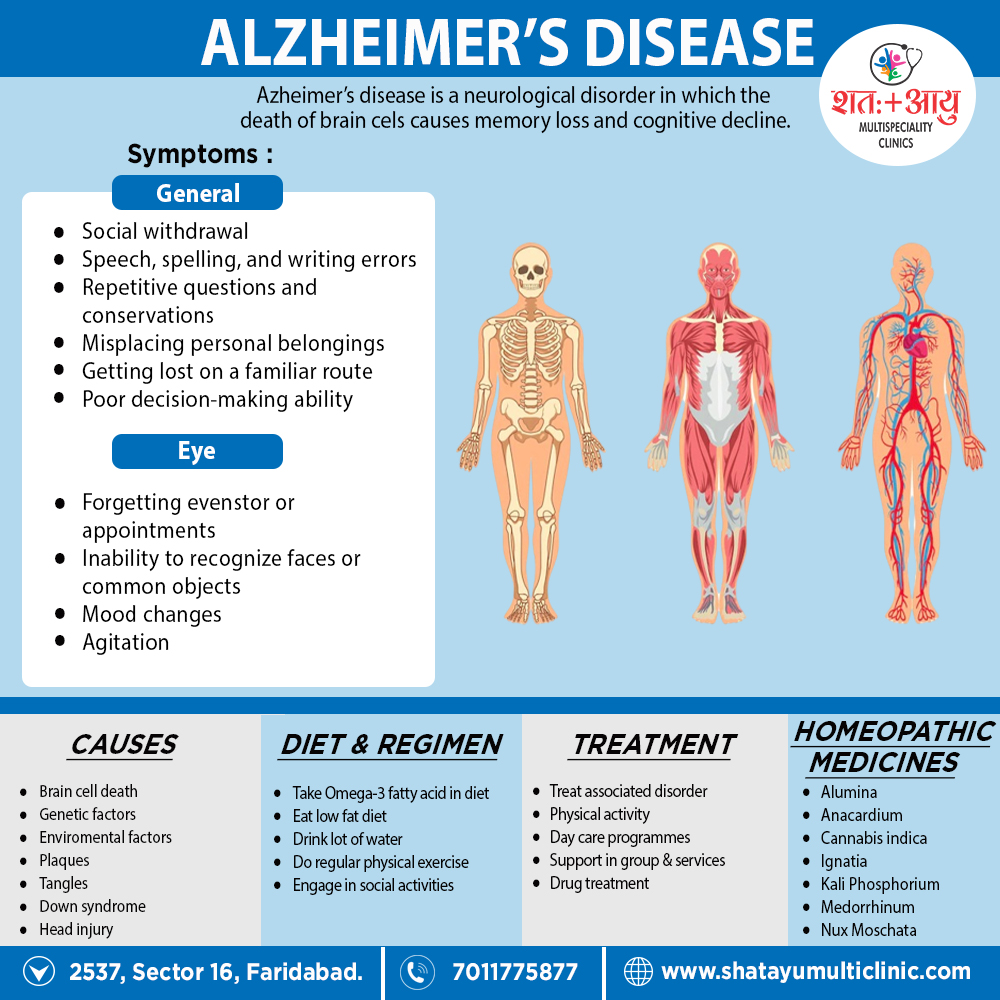
Homeopathic Medicines for Alzheimer’s Disease:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Recommended Homeopathic Treatment for Alzheimer’s disease:
- The popularly recommended homeopathic remedies for Alzheimer’s disease are Anacardium, Cannabis Indica, Medorrhinum, Ignatia and Kali Phos.
- Anacardium is a suitable remedy for marked forgetfulness. Additionally, Sudden diminution of memory of what a person has just seen, just listened to or names of people surrounding him appears.
- Cannabis Indica is the appropriate choice for short-term memory loss in persons with Alzheimer’s disease.
- Medorrhinum ranks high as a cure for memory loss for the names of well-known persons and places.
- Last medicines Ignatia and Kali Phos are wonderful remedies to deal with depression in Alzheimer’s patients.
1. Homeopathic medicines for Alzheimer’s disease with marked forgetfulness:
Effective homeopathic medicines for Alzheimer’s disease with marked forgetfulness are Anacardium and Alumina.
Anacardium:
- Anacardium is a good choice when the person is very forgetful.
- He forgets what he has seen and suddenly forgets names of people surrounding him.
- Memory progressively gets bad.
- Along with forgetfulness, the person also shows irritability, anxiety, anger with violent behavior and use of foul language.
Alumina:
- It is also a valuable selection for forgetfulness in Alzheimer’s disease.
- Alumina is selected when memory is weak or entirely lost.
- The person has cloudiness in the mind, he is slow to answer and lacks judgement power.
- Absent mindedness also prevails.
- He also makes mistakes while writing and speaking.
2. Homeopathic medicines for Alzheimer’s disease with short term memory loss:
Cannabis Indica:
- Cannabis Indica is one of the best homeopathic remedies for Alzheimer’s disease with short-term memory loss.
- It is indicated where a person forgets frequently while he is doing a specific task or soon after doing it.
- He forgets what he has just done, or what has just happened, or what he has just said or read.
- He also forgets what he is about to do, what he is about to write.
- Forgets frequently while talking.
- While speaking a sentence, he forgets what he is about to say, forgets the words in his mouth.
- Sudden loss of ideas and speech also appears. He begins a sentence but cannot finish it.
- There is inability to recall ideas even after exerting the mind to do so.
3. Homeopathic medicines for Alzheimer’s disease with loss of memory for names of well-known persons and places:
Medorrhinum:
- Medorrhinum is among the top-grade homeopathic remedies for Alzheimer’s disease where a person shows loss of memory for names of well-known persons and places.
- Surprisingly, He forgets names of close friends and family members.
- Eventually, In extreme cases, he even forgets his own name.
- Medorrhinum is also indicated when a person finds it difficult to carry on a conversation.
- He gets lost while conversing and a question has to be repeated.
- He is unable to collect ideas also gives incorrect replies.
4. Homeopathic medicines for Alzheimer’s disease with difficulty while reading and writing from memory weakness:
The prominently indicate homeopathic remedies for Alzheimer’s disease with weak memory posing a difficulty in reading and writing are i.e. Lac Caninum and Nux Moschata.
Lac Caninum:
- Lac Caninum is helpful when the person is forgetful while writing.
- He makes use of wrong words while writing, doesn’t remember appropriate words.
- He makes spelling mistakes, omit letters in words.
- While reading or writing, he is unable to concentrate.
- Person needing Lac Caninum seems hopeless about recovery.
- The person is sure that the disease is incurable also recovery is impossible.
Nux Moschata:
- Nux Moschata is prescribing for sudden vanishing of thoughts while reading or writing.
- Person uses wrong words either in reading or in writing.
- Moreover, He frequently makes a wrong selection of words.
- He may also show marked drowsiness, absent- mindedness and indifferent behavior accompanying the above symptoms.
5. Homeopathic medicines for Alzheimer’s disease to deal with accompanying depression and emotional imbalance:
The most appropriate homeopathic remedies for Alzheimer’s disease to deal with depression and emotional imbalance are i.e. Ignatia, Kali Phos and Aurum Met.
Ignatia:
- Ignatia is the best choice when a person experiences sadness, weeping spells, and desire to be alone.
- It is also indicated for mood swings.
Kali Phos:
- It can help when a person has marked exhaustion, fatigue, lassitude, and weariness along with Alzheimer’s disease.
- Kali Phos is also indicated for gloominess, despondency, sadness, and a dull mind accompanying Alzheimer’s disease.
Aurum Met:
- Aurum Met is useful when depression with suicidal tendencies persists in Alzheimer’s disease.
- A person requiring Aurum Met also feels he is worthless and of little importance, he feels life is a burden.
- Even the slightest contradiction is unbearable and leads to acute anger outbursts in such persons. [4]