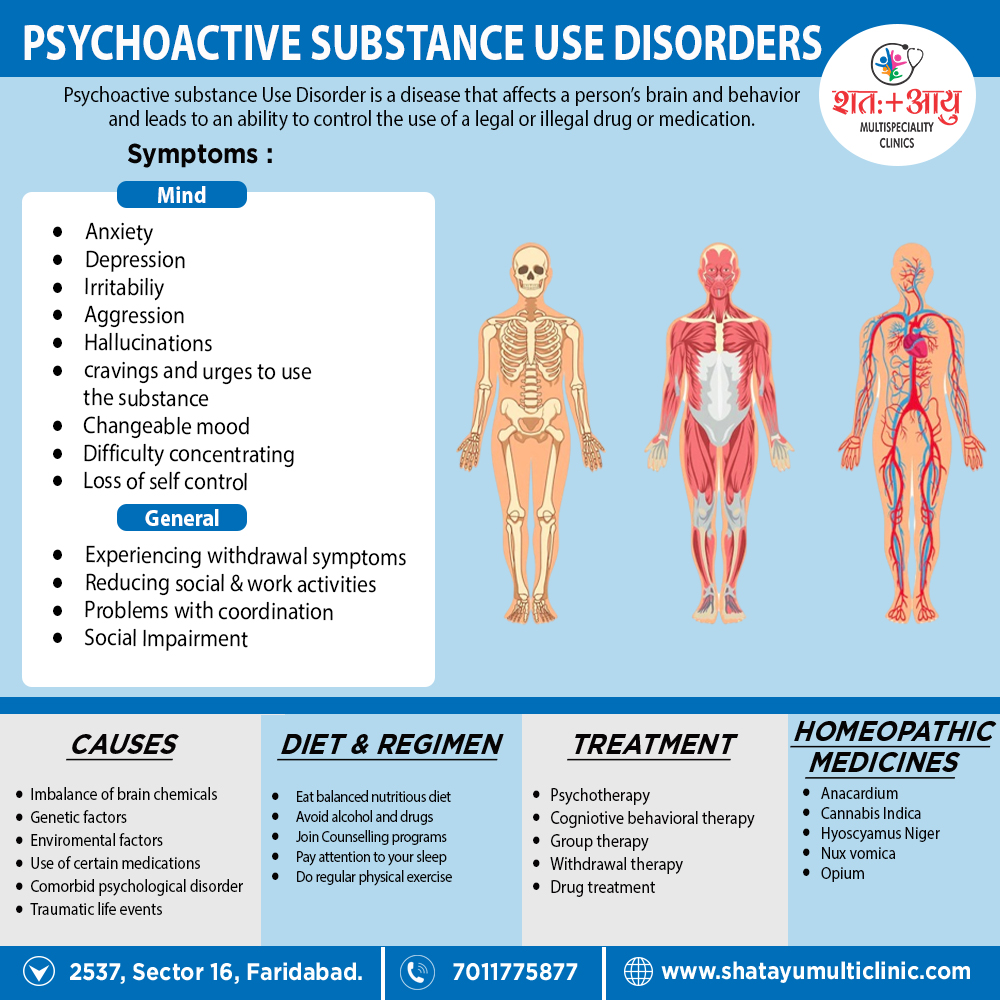
Overview of Psychoactive Substance Use Disorders:
The use of alcohol and other psychoactive substances has recorded throughout history, often with the primary aim of changing an individual’s mood or relieving the distress of harsh circumstances.
Early examples include the chewing of tobacco leaves or coca (cocaine) in North America and Peru, respectively.
Humans are clearly vulnerable to the desire to use substances; this is illustrate by the fact that alcohol and other psychoactive substances remain a leading cause of medical and social problems worldwide and cause psychoactive substance use disorders.
World Health Organization (WHO) statistics report that alcohol is the primary causative factor in 4 percent of the global burden of disease. [1]
Drug:
A drug is defined (by WHO) as any substance that, when taken into the living organism, may modify one or more of its functions. This definition conceptualises ‘drug’ in a very broad way, including not only the medic at ions but also the other pharmacologically active substances.
The words ‘drug addiction’ and ‘drug person with substance abuse disorder’ were dropped from scientific use due to their derogatory connotation. Instead ‘ drug abuse’, ‘ drug dependence’, ‘ harmful use’, ‘misuse’, and ‘psychoactive substance use disorders’ are the terms used in the current nomenclature.
A psychoactive drug is one that is capable of altering the mental functioning.
There are four important patterns of psychoactive substance use disorders, which may overlap with each other:
1. Acute intoxication
2. Withdrawal state
3. Dependence syndrome
4. Harmful use.
The other syndromes associated with the psychoactive substance use in ICD-10 include psychotic disorder, amnesic syndrome, and residual and late-onset (delayed onset) psychotic disorder.