Homeopathic Treatment of Pregnancy induced hypertension (Preeclampsia)
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
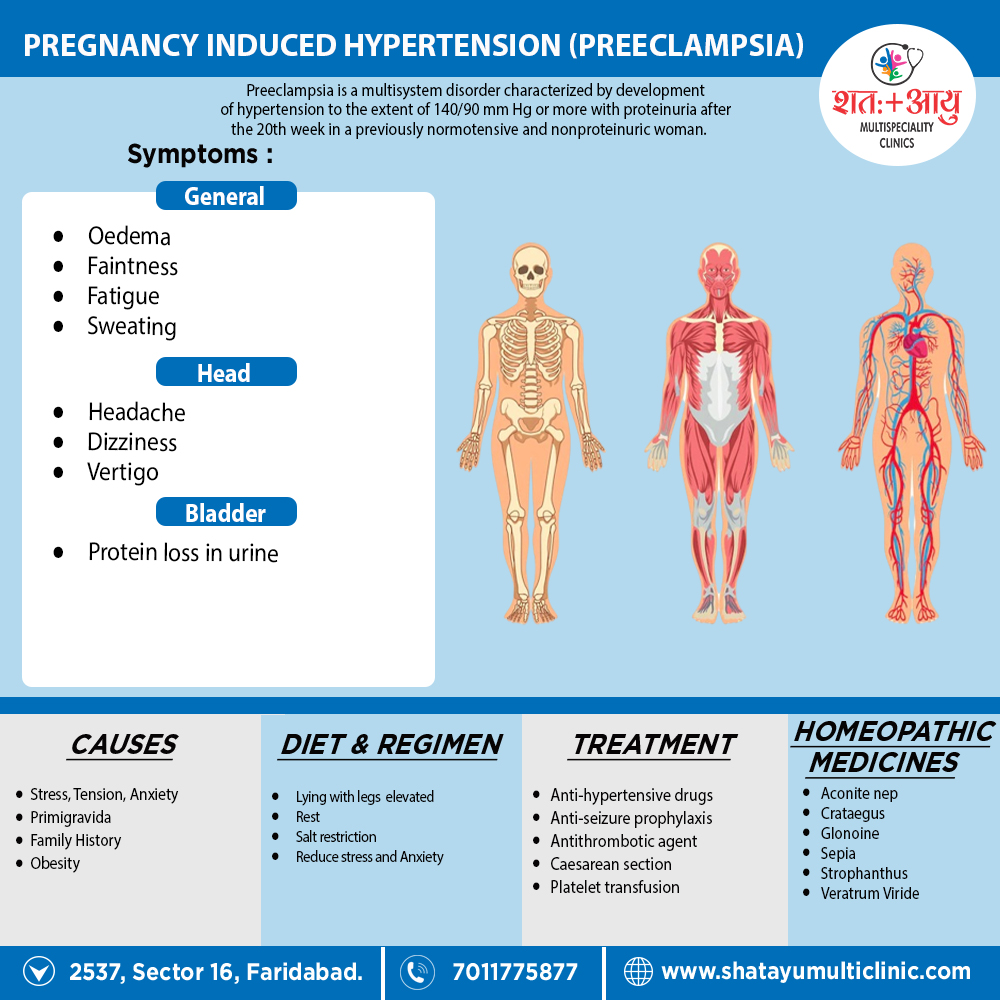
Homeopathic Medicines for Pregnancy induced hypertension (Preeclampsia)
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Aconite
- Intense anxiety, fear, restlessness and tossing about.
- Sudden, violent acute conditions, due to fright, shock, cold dry winds; getting chilled whilst sweating.
- Hyperpyrexia with burning thirst, hot dry skin and rapid pounding pulse. Profuse arterial hemorrhages.
- Numbness and tingling of affected parts.
- Congestions and inflammations with sweating, redness and burning.
- Better – warmth and after sweating.
Glonoine
- Confusion with dizziness.
- Head heavy but cannot lie it on a pillow, can’t bear anything about the head.
- Surging of blood to heart and head. Severe congestions to the head.
- Tendency to sudden and violent irregularities of the circulation.
- Any exertion brings rush of blood to heart and fainting spells. Pulsating sensation through’ body.
- Face flushed hot, livid; sweaty.
- Worse – in the sun, exposure to sun rays, gas open fire: jar, stooping, having hair out; peaches, stimulants, from 6am to noon, L side.[2]
Strophanthus Hispidus:
- Acts on the heart; diminishes the rapidity. Arteriosclerosis, rigid arteries of the aged.
- Restores tone to a brittle tissue, esp. heart muscle and valves.
Sepia:
- Irritable, easily offended. Sad, indifferent to those loved best. Averse to occupation, to family.
- Weakness, yellow complexion.
- Pulsating headache in cerebellum.
- Violent intermittent palpitation, Beating in all arteries.
- Tremulous feeling with flushes. Feet hot and hands cold and vice versa.
- Worse – standing. cold air, Forenoon, evenings, washing, dampness, L side, before thunderstorm.
- Better – exercise, press., warmth of bed, hot applications, after sleep.
Veratrum viride:
- Quarrelsome and delirious. Especially adapted to full blooded, plethoric persons. Additionally, Controls action of heart and pulse.
- Paroxysms of auricular fibrillation.
- Valvular diseases, Beating of pulse throughout especially in R thigh. Bloated livid face.
- Bloodshot eyes. Great prostration. Lastly, Narrow well developed streak right through the middle of the tongue.
Crataegus:
- Apprehensiveness and despondency.
- Heart tonic, Acts on heart muscle, Irregularity of heart.
- Insomnia of aortic sufferers; Oedema. High arterial tension.
- Sedative to cross, irritable patients.
- Arteriosclerosis; said to have a solvent power upon crustaceous deposits in arteries.
- Extreme Dyspnoea on least exertion, without much increase in pulse.
- Worse – warm room. Better – fresh air, quiet and rest.[2]