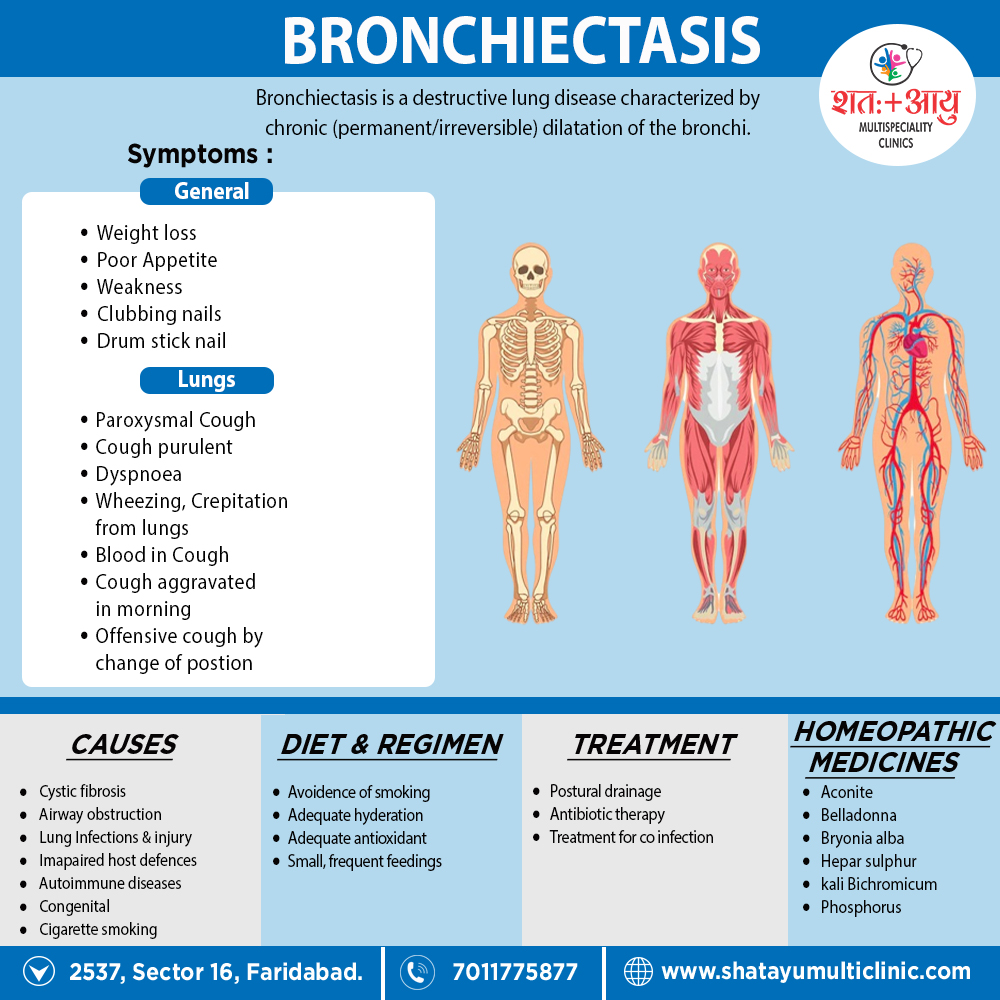
In detail, there are many causes that can induce or contribute to the development of bronchiectasis. The frequency of these different causes varies with geographic location. Additionally, Cystic fibrosis identifies as a cause in up to half of cases. Bronchiectasis without CF is known as non-CF bronchiectasis. Historically, about half of all case of non-CF bronchiectasis were found to be idiopathic, or without a known cause. However, more recent studies with a more thorough diagnostic work-up have found an etiology in 60 to 90% of patients.
Cystic fibrosis
Cystic fibrosis is the most common life-threatening autosomal recessive disease in the United States and Europe. It is a genetic disorder that affects the lungs, but also the pancreas, liver, kidneys, and intestine. In general, It cause by mutations in the CFTR protein, a chloride channel expressed in epithelial cells. Lung disease results from clogging of the airways due to mucus build-up, decreased muco-ciliary clearance, also resulting inflammation. In later stages, changes to the structure of the lung, such as bronchiectasis, occur. Around 5 to 10% of all patients with cystic fibrosis develop bronchiectasis.
Airway obstruction
An airway obstruction can cause by either an intraluminal mass such as a tumor or a foreign body. Furthermore, the presence of an airway obstruction leads to a cycle of inflammation. It is important to identify the presence of an obstruction because surgical resection is often curative if obstruction is the cause. In adults, foreign body aspiration often associate with an altered state of consciousness. The foreign body often unchewed food, or part of a tooth or crown. In conclusion, Bronchiectasis that results from foreign body aspiration generally occurs in the right lung in the lower lobe or posterior segments of the upper lobe.
Lung infections
A range of bacterial, mycobacterial, also viral lung infections are associated with the development of bronchiectasis. Bacterial infections commonly associated with bronchiectasis i.e. P. aeruginosa, H. influenzae, and S. pneumoniae. Gram-negative bacteria more commonly implicate than gram-positive bacteria. A history of mycobacterial infections such as tuberculosis can lead to damage of the airways that predisposes to bacterial colonization. In brief, Severe viral infections in childhood can also lead to bronchiectasis through a similar mechanism. Nontuberculous mycobacteria infections such as Mycobacterium avium complex found to be a cause in some patients. Lastly, Recent studies have also shown Nocardia infections to implicated in bronchiectasis.
Impaired host defences
Impairments in host defenses that lead to bronchiectasis may be congenital, such as with primary ciliary dyskinesia, or acquired, such as with the prolonged use of immunosuppressive drugs. Additionally, these impairments may localized to the lungs, or systemic throughout the body. In these states of immunodeficiency, there a weakened or absent immune system response to severe infections that repeatedly affect the lung and eventually result in bronchial wall injury. HIV/AIDS an example of an acquired immunodeficiency that can lead to the development of bronchiectasis.
Aspergillosis
Allergic bronchopulmonary aspergillosis (ABPA) an inflammatory disease caused by hypersensitivity to the fungus Aspergillus fumigatus. It suspected in patients with a long history of asthma also symptoms of bronchiectasis such as a productive, mucopurulent cough. Imaging often shows peripheral and central airway bronchiectasis, which unusual in patients with bronchiectasis caused by other disorders.
Autoimmune diseases
Several autoimmune diseases have associated with bronchiectasis. Specifically, individuals with rheumatoid arthritis and Sjogren syndrome have increased rates of bronchiectasis. In these diseases, the symptoms of bronchiectasis usually present later in the disease course. Other autoimmune diseases such as ulcerative colitis and Crohn’s disease also have an association with bronchiectasis. Additionally, graft-versus-host disease in patients who have underwent stem cell transplantation can lead to bronchiectasis as well.
Lung injury
Bronchiectasis could caused by: inhalation of ammonia and other toxic gases, chronic pulmonary aspiration of stomach acid from esophageal reflux or a hiatal hernia.
Congenital
Bronchiectasis may result from congenital disorders that affect either cilia motility or ion transport. A common genetic cause cystic fibrosis, which affects chloride ion transport. Another genetic cause is primary ciliary dyskinesia, a rare disorder that leads to immotility of cilia and can lead to situs inversus. When situs inversus accompanied by chronic sinusitis and bronchiectasis, this known as Kartagener’s syndrome. Other rare genetic causes include Young’s syndrome and Williams-Campbell syndrome.
Tracheobronchomegaly, or Mourner-Kuhn syndrome a rare condition characterize by significant tracheobronchial dilation and recurrent lower respiratory tract infections. Individuals with alpha 1-antitrypsin deficiency have found to be particularly susceptible to bronchiectasis, due to the loss of inhibition to enzyme elastase which cleaves elastin. This decreases the ability of the alveoli to return to normal shape during expiration.
Cigarette smoking
A causal role for tobacco smoke in bronchiectasis has not demonstrated. Nonetheless, tobacco smoking worse pulmonary function and accelerate the progression of disease that is already present