Overview
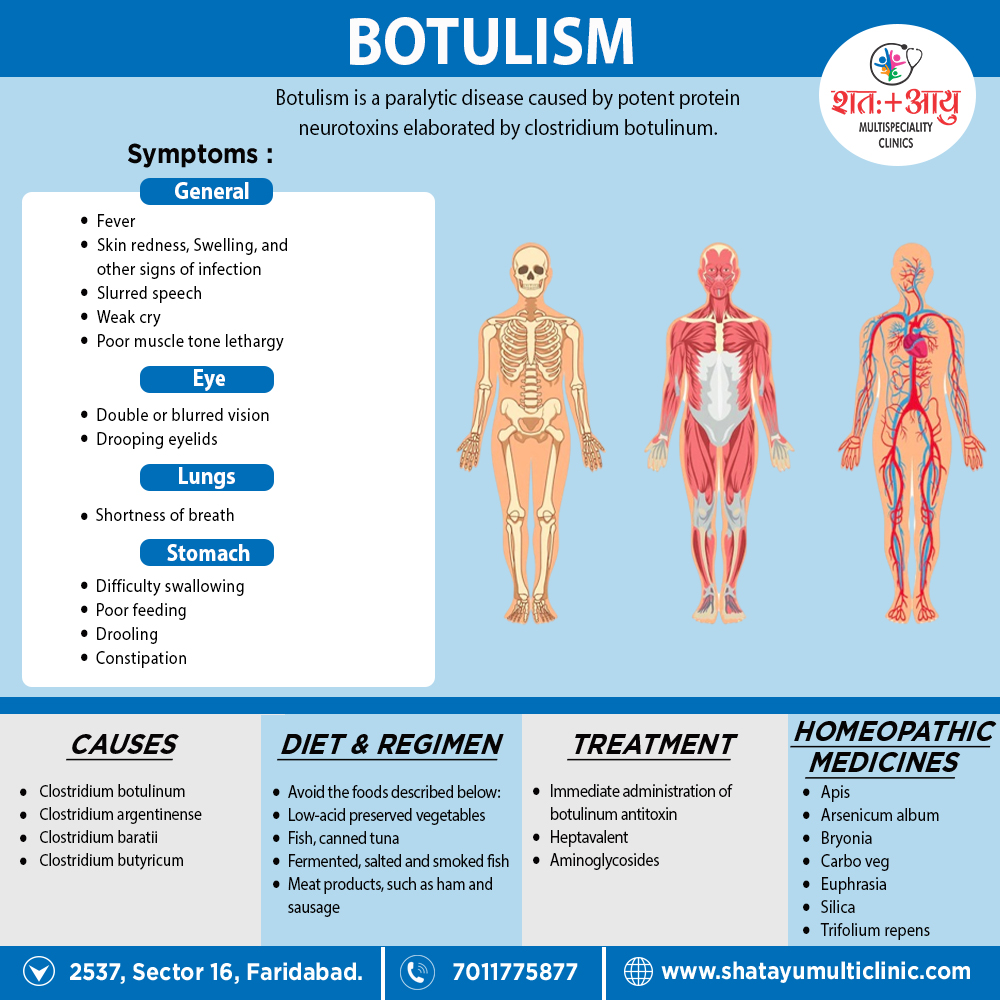
Botulism, recognized at least since the eighteenth century, is a neuroparalytic disease cause by botulinum toxin, one of the most toxic substances known. While initially thought to cause only by the ingestion of botulinum toxin in contaminated food (food-borne botulism), three additional forms cause by in situ toxin production after germination of spores in either a wound or the intestine are now recognized worldwide: wound botulism, infant botulism, and adult intestinal colonization botulism.
In addition to occurring in these recognized natural forms of the disease, botulism symptoms have report in patients receiving injections of botulinum toxin for cosmetic or therapeutic purposes (iatrogenic botulism). Moreover, botulism was reported after inhalation of botulinum toxin in a laboratory setting.
Spread of Botulism
All forms of botulism manifest as a relatively distinct clinical syndrome of symmetric cranial-nerve palsies followed by descending bilateral flaccid paralysis of voluntary muscles, which may progress to respiratory compromise and death. The mainstays of therapy are meticulous intensive care and treatment with antitoxin as soon as botulism is suspected and before other illnesses have been ruled out.[1]
Botulism occurs worldwide, but the number of cases reported varies among countries and regions.
The variation may be due not only to actual differences in incidence but also to
(1) availability of resources to identify botulism, a rare disease
(2) differences in reporting requirements
(3) limited external access to data collections
There is no universal surveillance system to capture worldwide botulism incidence. However, 30 countries currently participate in voluntary reporting of botulism cases to the European Union through an established surveillance system that includes standardized case definitions similar to those used in the United States and Canada. Other countries (e.g., Argentina, China, Thailand, Japan) maintain independent botulism surveillance. [1]