Homeopathic Treatment of Chronic obstructive pulmonary disease
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
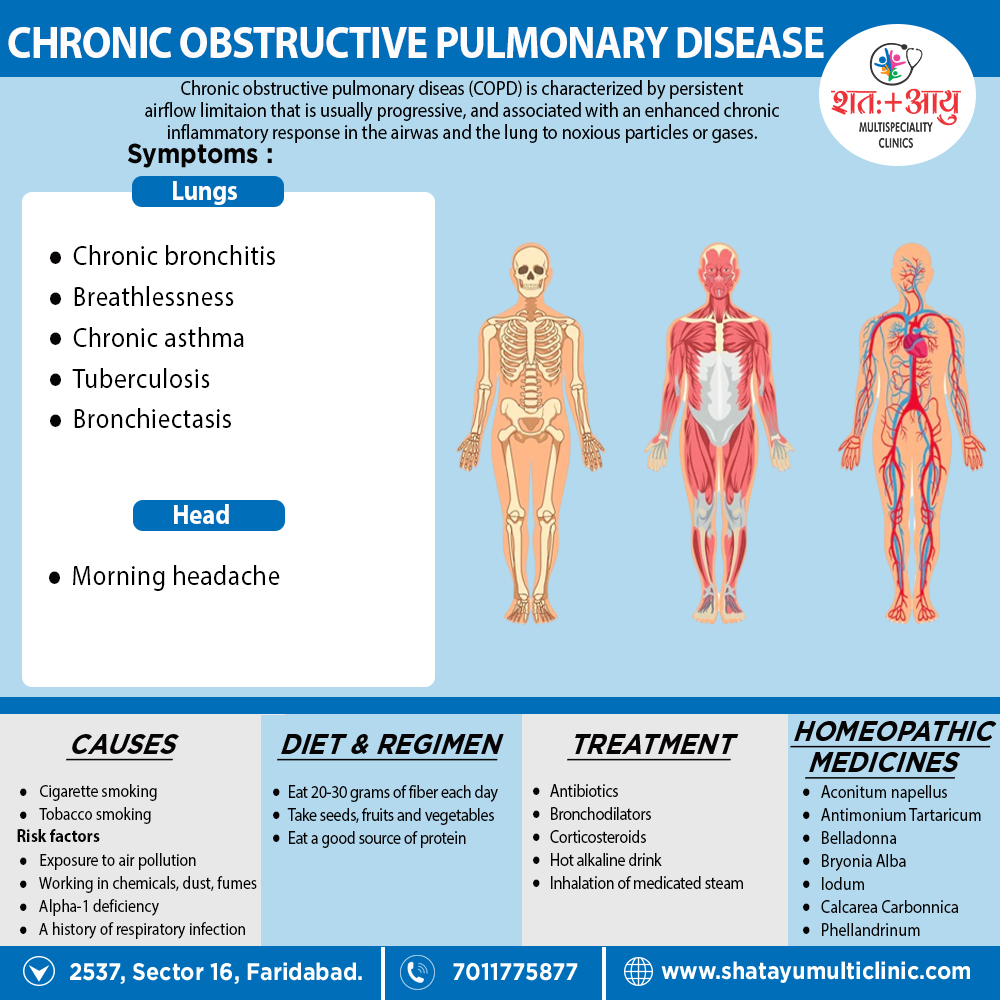
Homeopathic Medicines for Chronic obstructive pulmonary disease :
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Homoeopathic Approach:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’.
The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Medicines:
1.Aconitum Napellus:
- The first remedy that is often indicated at the onset of the infection. It is effective only within the first twenty-four hours.
- Useful when there is a short, dry cough, a temperature and an irritation of the throat, chest and trachea.
- There is a chilly restlessness, anxiety and a full, bounding pulse, with general weakness.
2. Antimonium Tartaricum:
- Useful when there is a accumulation of considerable loose, rattling, moist mucus in the chest.
- For children breathing and a loose cough, but little phlegm is expectorated.
- There may be vomiting and labored breathing. Pronounced physical and mental exhaustion.3. Belladona:
- A high temperature, dry cough, a pounding, pulsating headache and a flushed face with a dry, hot skin.
- The cough is worse at night and when lying down.4. Bryonia Alba:
- A painful, violent, dry, stitching cough with a headache and pain in the chest wall.
- Worse with coughing and better when supporting the area with both hands.
- The expectoration is yellow and often blood streaked. The cough is worse after meals.
- Patient drinks large quantities of fluids at long intervals.5. Iodum:
- Difficult expansion of chest, blood-streaked sputum; internal dry heat, external coldness.
- Inspiration difficult. Croupy cough with difficult respiration; wheezy.
- Cold extends downwards from head to throat and bronchi. Great weakness about chest.
- Palpitation from the least exertion. Iodum cough.6. Calcarea carbonica:
- Extreme Dyspnoea. Suffocating spells, tightness, burning and soreness in chest.
- Chest very sensitive to touch, percussion or pressure. Longing for fresh air.
- Bloody expectoration.7. Phellandrinum:
- Respiratory remedy. Good remedy for offensive expectoration and cough phthisis.
- Tuberculosis, affecting generally the middle lobes. Everything tastes sweet.
- Dyspnoea and continuous cough early in morning.
- Cough, with profuse and fetid expectoration; compels him to sit up. Hoarseness.[3]